Hepatitis: Treatment, Nutrition, and Essential Medical Information
What differentiates types of hepatitis, and is there a vaccine for them? How does jaundice differ from hepatitis, and when does the condition become chronic?
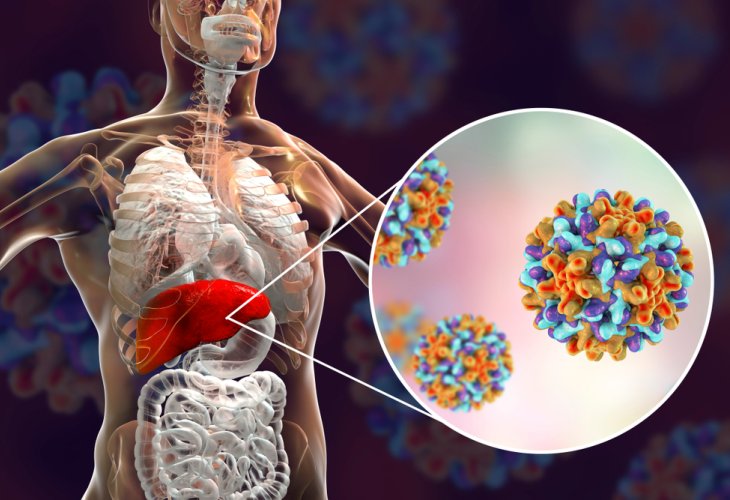 (Photo: Shutterstock)
(Photo: Shutterstock)It is somewhat known as "jaundice," due to bilirubin accumulation leading to yellowing of the skin and eyes. However, hepatitis is actually liver inflammation, with jaundice being just one of its symptoms.
(Not) Nice to Meet: What is Hepatitis?
Hepatitis is a digestive system disease, commonly caused by hepatitis viruses and, less frequently, by metabolic damage or overconsumption of alcohol or drugs.
Viral hepatitis is divided into several types and subtypes, with the most common being hepatitis A, hepatitis B, and hepatitis C.
Hepatitis A is caused by the hepatitis A virus. This contagious disease primarily affects children, who usually endure it as a mild childhood illness, sometimes without any symptoms. When contracted by young or older adults, it presents more severely and often results in complications, potentially leading to severe liver failure – a rare occurrence in young patients but present in about 80% of older individuals. Those who recover are immune for life.
Currently, the hepatitis A virus is mainly prevalent in developing countries with low hygiene levels. A hepatitis A vaccine is now part of routine childhood vaccinations, making the virus almost nonexistent in Israel and other developed countries. A preventive vaccine is also available for travelers to regions where the virus is common.
Hepatitis B arises from the hepatitis B virus, and spreads through secretions or skin-penetrating contact (for example, using non-sterile needles, etc.). An infected mother may pass the disease to her newborn during childbirth. Typically, the illness resolves after its onset, similar to hepatitis A, but sometimes it becomes chronic. The younger the patient, the higher the risk of developing chronic disease.
Today, this disease, too, is preventable through infant vaccinations, thus it is rare.
Hepatitis C, in contrast, is the only common type of hepatitis without a vaccine as of now. Hepatitis C spreads through exposure to blood contaminated with the virus. People who received blood transfusions before 1992 are at higher risk for contracting hepatitis C, as testing for the virus in blood donations only began in that year.
Hepatitis C can exist in the host's body for many years without symptoms. The virus is not "dormant," as with other types of viruses, but active – without causing immediate damage or symptoms. However, after years of carrying, significant liver damage may occur, leading to hepatitis symptoms. Hepatitis C is a chronic disease requiring close and long-term medical monitoring. Early identification of the virus may allow for effective medical treatment to eradicate the virus completely.
Diagnosis: How Do I Know if I Have Hepatitis?
Hepatitis, in all its forms, presents similar symptoms, some resembling the flu: fatigue and weakness, abdominal pain and vomiting, sometimes diarrhea, loss of appetite, joint pain, and occasionally fever. Later, jaundice symptoms can appear – a yellowish tint to the skin and the sclera of the eyes, and darker urine. Medical examination may also show liver enlargement. The more advanced the disease and the greater its liver impact, the more prominent the symptoms will be, some only appearing when hepatitis complications arise, such as cirrhosis (liver tissue destruction and replacement with connective tissue). If left untreated and severe cirrhosis develops, brain damage may occur, leading to symptoms like intellectual impairment, personality changes, and even loss of consciousness.
If any symptoms arise that suggest hepatitis virus infection, diagnosis is made via a simple blood test to detect the virus.
For hepatitis C, more prevalent today, its carriers often go undiagnosed until significant disease outbreaks, as it remains asymptomatic in the body. Virus detection may occur incidentally during other blood tests. Sometimes, it's identified early in disease onset through symptom awareness.
 (Photo: Shutterstock)
(Photo: Shutterstock)
So I Have Hepatitis. What's Next?
Here we will focus on treatment for hepatitis C, the most common type today. Hepatitis treatment is administered by a gastroenterologist specializing in the liver. Treatment for hepatitis C is not automatic; sometimes, no treatment is necessary. Treatment decisions depend on factors like virus levels in the blood, existing liver damage, and the patient's overall health. When treatment is needed, a mix of antiviral drugs is used. Treatment lasts several weeks to months, with ongoing evaluations to assess effectiveness. Different types of treatment are available, allowing regimen changes if one proves ineffective. Severe side effects, like weakness, anemia, and fever, may also prompt treatment changes. No matter the case, the treatment is intensive and conducted under strict medical supervision.
The goal of hepatitis C treatment is to prevent liver damage or limit existing damage expansion and, ideally, eliminate the virus completely. Treatment cannot repair damage already done to the liver.
Individuals in the quiet phase of the disease, where the virus is inactive, need to maintain a particularly healthy lifestyle. Maintaining a healthy weight, avoiding smoking, and engaging in regular physical activity are advised. Hepatitis carriers are particularly advised against alcohol consumption—as it can exacerbate liver damage.
As mentioned, the disease may reveal itself at different stages. From diagnosis onwards, consistent and organized medical follow-up is crucial, along with regularly taking prescribed medications and staying alert to any health changes or symptoms that may indicate hepatitis complications—like fever, significant weakness, unfamiliar abdominal pain, changes in discharge color, etc.
Nutrition: What Should I Eat if I Have Hepatitis?
As stated, hepatitis patients are strongly encouraged to maintain a healthy lifestyle. While a healthy diet alone cannot cure hepatitis, it can certainly slow chronic hepatitis progression and enhance the patient's quality of life. Staying on a low-fat diet is important to prevent fatty liver conditions. Fatty liver is common among people due to obesity or excessive alcohol consumption and can worsen the progression of other liver diseases—including, of course, all types of hepatitis.
Thus, hepatitis patients are advised to completely avoid alcohol and fatty meats—like lamb, fatty beef, or ground beef (burgers, sausages, etc.). Fish, chicken, and turkey without skin are recommended. Fried foods of all kinds should also be avoided. Foods high in fat, such as butter and margarine (and meals containing them), should be avoided, as should coconut, which contains high levels of saturated fat.
Additionally, avoiding foods high in sugar is advised.
Hepatitis patients are advised to divide their nutrition into several small meals throughout the day, preferring it over large, complete meals. Regarding fruit, it's recommended to eat up to two servings a day—but not all at once, rather spread throughout the day, between meals.
Regular physical activity is also important, as mentioned, to slow the disease's progression, and close medical monitoring is essential for any dietary or treatment changes.

