Multiple Sclerosis: Treatment Options, Nutrition, and Essential Medical Information
What is multiple sclerosis, and where is it actually 'multiple'? How is the disease diagnosed, and what can you do to live a healthy life even with the disease? Everything you need to know.
 (Photo: shutterstock)
(Photo: shutterstock)Around 6,000 people in Israel and about 3 million globally suffer from a disease known as "Multiple Sclerosis." Despite its recognizable name, the symptoms, causes of onset, and treatment methods are less widely known. Let's try to clarify some things.
(Un)happy to Meet: Multiple Sclerosis
Multiple Sclerosis, or its English name Multiple Sclerosis, belongs to the group of autoimmune diseases—meaning diseases where the body attacks itself in one way or another. Multiple Sclerosis is a chronic inflammatory disease, and it is considered neurological—meaning it affects the central nervous system in the brain, spine, and spinal cord.
 (Photo: shutterstock)
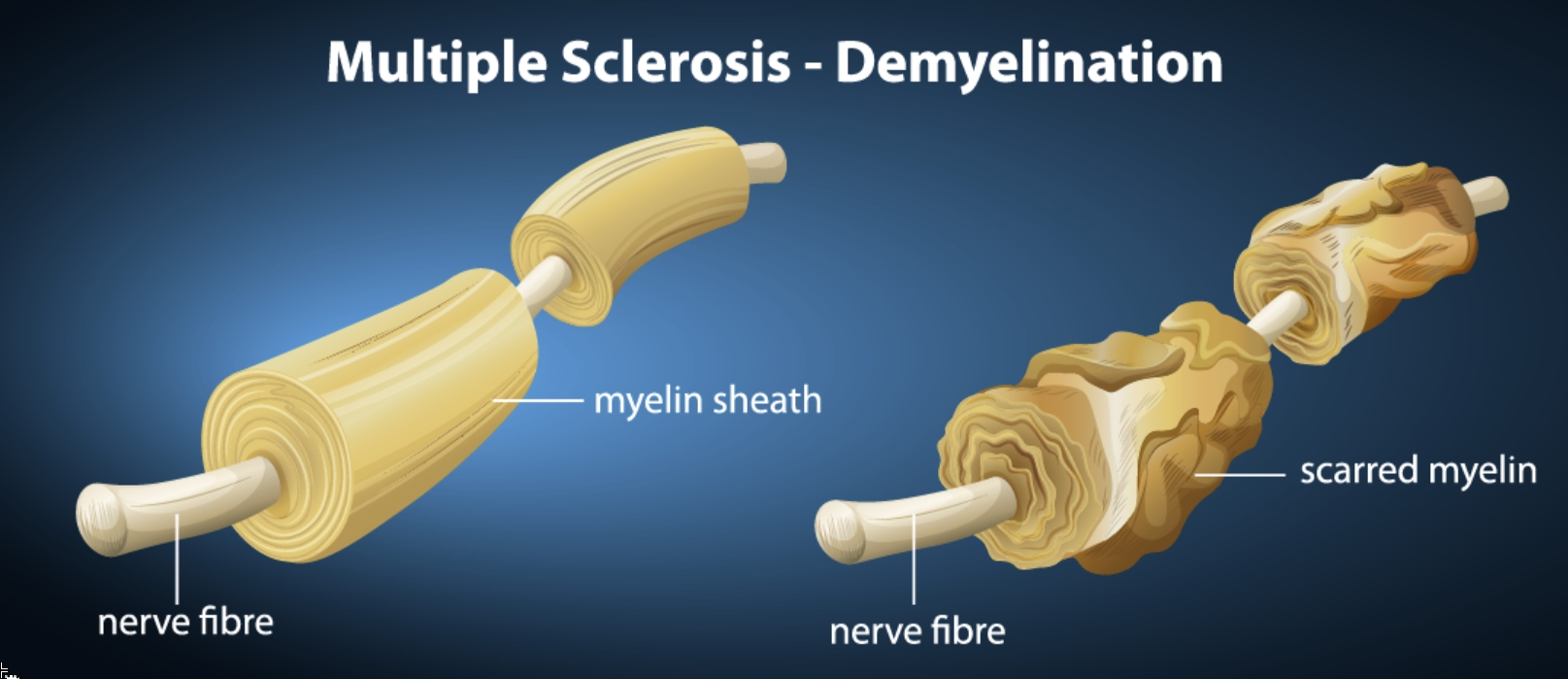
(Photo: shutterstock)The extensions of nerve cells throughout the body are coated by a protein called myelin, which plays an important role in the communication between nerves and assists in the proper functioning of the entire nervous system. In the case of Multiple Sclerosis, the body's immune system attacks the myelin, leading to the formation of sclerosis—scars in healthy tissue—within the central nervous system. The term "multiple" in the disease's name does not imply it is particularly common, but describes the disease's nature—the sclerotic tissues are widespread throughout all parts of the central nervous system.
Multiple Sclerosis appears mainly between the ages of 18-40, and its prevalence in women is twice as high as in men. The reason for this—as well as the reason for the disease's occurrence in general—is unknown. Hypotheses about the causes include a combination of some immune system disruption, genetic factors, and exposure to infections—mainly smoking. There is also some connection to vitamin deficiency.
In Israel, the "Israel Multiple Sclerosis Society" operates, providing information and assistance to patients and their families.
Diagnosis: How Will I Know If I Have Multiple Sclerosis?
Diagnosing Multiple Sclerosis often takes a long time, sometimes years. The reason is that its symptoms, especially in the early stages, are very minor and sometimes not felt at all. The symptoms also vary from person to person because they depend on the location of the nervous system that’s affected, as well as the severity of the disease. Common symptoms include increased fatigue, mood changes, frequent urination, instability while walking, some visual impairment, a tingling sensation, sensory disturbances, and hand weakness. As you can see, and considering that not all symptoms usually appear in everyone, these symptoms are quite common, and each of them—or even several together—can result from many other diseases, as well as complex mental health conditions. Therefore, it is not always recognized as a more significant illness.
It's important to note that Multiple Sclerosis has three main subtypes, and the differences among them also affect the symptoms. The first and most common type (85% of patients) is Relapsing-Remitting MS (RRMS)—a form where disease attacks occur, with symptoms lasting for several days or more, followed by a remission period during which symptoms diminish, or even disappear completely for an interval. The second type is Secondary Progressive MS (SPMS), where after an attack, there is no remission, and symptoms continue or even worsen. About half of those suffering from the first type of the disease who do not receive drug treatment will experience a progression to the second type over the next ten years. The third type is Primary Progressive MS (PPMS), where there are no attacks, but persistent symptoms that gradually worsen.
When there is suspicion that a patient suffers from Multiple Sclerosis, several diagnostic tools are used to identify the disease. Regular blood tests do not provide answers for diagnosis, so more comprehensive tests are needed. However, comprehensive blood tests are usually conducted before diagnosis to rule out other, more common causes for the existing symptoms. The diagnosis is generally performed through an MRI scan, which images both the brain and the spinal cord. In cases of Multiple Sclerosis, the scan can reveal lesions typical of the disease. Occasionally, when the scan results are not sufficient for a clear diagnosis, a lumbar puncture is performed—by extracting a small amount of fluid from the spinal canal using a needle inserted between two vertebrae in the lumbar spine. Examining this fluid can definitively identify Multiple Sclerosis.
So I Have Multiple Sclerosis. What's Next?
As of today, there is no cure for Multiple Sclerosis. However, unlike in the past, there are now numerous treatments that slow disease progression and allow a continued quality of life alongside the disease. Treatment is divided into four main parts.
In cases of severe attacks, treatment is typically done with intravenous steroid administration for several days.
During non-severe attacks, symptomatic treatment is available to alleviate various disease symptoms, tailored to existing symptoms—such as pain relief, medications to help muscle stiffness, and more.
Between attacks, immunomodulatory treatment can assist. This treatment aims to reduce the frequency of attacks and slow disease progression, as noted. Currently, there is a very wide range of possible medications for treatment. In consultation with a neurologist handling the disease, patients can find the appropriate treatment. Some medications are administered intravenously, others by injection or as pills. The choice between various medications depends on the course of the disease, its progression rate, and the patient's personal preferences, making open communication with the treating doctor crucial to tailoring the right and most effective medications.
 (Photo: shutterstock)
(Photo: shutterstock)The last part of treatment includes physical therapy, occupational therapy, and other forms of physical activity. This part is very important and also takes place between attacks and in the long term. The aim of these treatments is to maintain body flexibility and the patient’s range of motion, allowing them to maintain a healthy routine as much as possible.
If you have been diagnosed with Multiple Sclerosis, it is important to try to maintain as normal and healthy a lifestyle as possible. Regular physical activity is especially important, and at the same time—ensuring adequate sleep and suitable rest. It is even more important for Multiple Sclerosis patients than for any other individuals to avoid smoking, which can exacerbate disease progression, and it is advisable to ensure as balanced and healthy a diet as possible.
You should know that women diagnosed with Multiple Sclerosis can conceive and give birth. The disease itself does not affect the fetus and does not harm it. However, some medications used to treat Multiple Sclerosis can harm the fetus. Therefore, it is important to plan for pregnancy in coordination with the treating doctor, and try as much as possible to begin a pregnancy when the disease is balanced. When the disease is balanced, it may sometimes be possible to discontinue medications harmful to the fetus even before pregnancy. If medication is still needed, alternative medications that do not affect the fetus can be used. It is worth noting that during pregnancy itself, there is a decreased tendency for disease attacks, but in the three to four months following delivery, there is an increased risk of attacks—especially in women whose disease was active before pregnancy began. Attention should be paid to the possibility of using medications that do not also affect breastfeeding. In most cases, women with Multiple Sclerosis can breastfeed without special problems.
Nutrition: What Should I Eat If I Have Multiple Sclerosis?
Unfortunately, there is no "miracle diet" that can help cure or balance Multiple Sclerosis. It is important to maintain a balanced and healthy diet, as recommended for any healthy person, to support overall body health and assist in the balance of the disease.
Nevertheless, Multiple Sclerosis experts provide a few recommendations to emphasize. Experts believe that a diet low in fat and high in fiber can be beneficial. Therefore, specific recommendations for Multiple Sclerosis patients include avoiding saturated fats as much as possible, and instead consuming healthy fats—like fatty fish (mackerel, tuna, or salmon), cheese, egg yolks, beef liver, and more. It is also recommended to consume foods containing vitamin D, and if necessary, take it as a dietary supplement.
For patients experiencing urinary issues, it is advised to avoid drinks containing aspartame, caffeine, or alcohol, which can increase sensitivity.
Another important nutritional consideration is gluten. Gluten consumption does not affect the development of Multiple Sclerosis or its progression. However, some studies show that Multiple Sclerosis patients have a higher percentage of gluten intolerance compared to the general population. This does not mean Multiple Sclerosis patients should automatically avoid gluten—but it may be worthwhile to pay attention to additional symptoms and to detect gluten intolerance early, if it exists.

